A new approach to retinal imaging developed at the University of Pittsburgh could lead to earlier diagnoses of eye diseases like glaucoma. The technique provides a detailed picture of the back of the eye, which could help ophthalmologists determine the health of cells essential for vision.
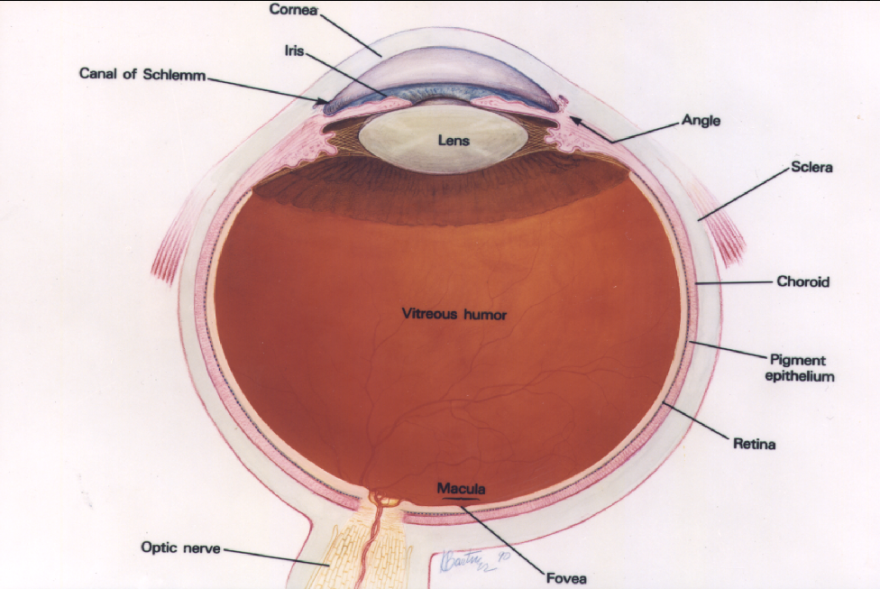
Vision occurs when particles from light, called photons, bounce off objects and enter the eye. They first pass a series of transparent layers, including the cornea, the lens behind the pupil and the vitreous body.
Assistant professor of ophthalmology Ethan Rossi said the new study,published in the Proceedings of National Academy of Sciences, will most directly impact the final stage of sight: the photon’s encounter with the retina.
Rossi said conventional methods used to image the retina used a technology called adaptive optics scanning laser ophthalmoscopy (AOSLO). To obtain the image, light is sent through the eye to the retina through the pupil, illuminates the region and bounces back toward the machine. The light is then recorded into a detector, which produces an image of the eye.
“Rods and cones, those cells are easy to see usually because they’re designed to absorb light,” Rossi said. “That also allows them to scatter light back out of the eye.”
Rods and cones are types of photoreceptors that work in the retina to process images and send pulses through the optic nerve to the brain.
The difficultly, according to Rossi, is gathering information about the class of cells that sit in front of the photoreceptor cells. These are the retinal ganglion cells (RGCs). RGCs are primarily responsible for relaying information to the brain.
“Those cells are transparent and they also don’t scatter a lot of light, which is great for vision, but it makes them really hard to image,” Rossi said.
The death or damage of RGCs can cause diseases like glaucoma. Previously, Rossi said the health of RGCs was determined by measuring the thickness of the retina over time.
“You need to have many, many of those cells, tens of thousands or maybe hundreds of thousands, be lost before you can detect a change,” Rossi said. “With this technique, we can go in and potentially see the loss of single cells or maybe even we can see changes in the cells before the cells are even lost.”
The new technique captures multiple images of the reflected light from multiple angles by varying the size and location of the detectors. The method is the first of its kind to use one detector in multiple positions to produce the comprehensive image. In the past, the detector cameras were placed along the optical axis and collected light.
“When we offset that detector, we were able to detect other light that’s scattered around in the eye off of multiple surfaces,” Rossi said. “That is what allows us to see other features that had previously been invisible.”
Researchers took multiple images from the different perspectives and combined them into a detailed, comprehensive picture of the eye. Ophthalmologists, Rossi said, can take these images and identify potential problem regions in patient eyes.
“We may eventually be able to see when these cells are sick and, if treatments are available, restore the health of those cells,” Rossi said. “We may be able to repair them before vision is lost.”
Offset axis imaging is not a new concept, according to Rossi. He said researchers have been adjusting microscope techniques, like focal plane range and aperture size, and applying them to ophthalmology since the 1990s.
"Next we have to figure out how to more efficiently harvest that light," Rossi said. "The sequential approach, where we're just moving this one detector to multiple locations, it takes a long time."
Before the research can enter clinical trials, Rossi said time it takes to scan the eye with his multi-offset approach needs to be cut by at least five or 10 minutes.
Much of the research was conducted at the University of Rochester, where Rossi worked until he moved to Pitt in August. He said the facilities are still working together and he hopes to start imaging his own patients as soon as renovations to the Pitt Ear and Eye Institute are complete.
In the meantime, Rossi said he's looking for investors to commercialize the technology in some way, which would bring it to the public sooner.
The study was funded by National Institutes of Health grants, Canon, Inc., Edward N. and Della L. Thome Memorial Foundation, and a grant from the University of Rochester Department of Ophthalmology from Research to Prevent the Blindness, New York, N.Y.





